The ROSC medical abbreviation stands for the return of spontaneous circulation and is the goal of cardiopulmonary resuscitation (CPR). When ROSC occurs, it means the patient’s body has resumed sustained cardiac activity, allowing for appropriate circulation to continue without additional CRP at that time.
What Are the Signs of ROSC?
When cardiovascular function begins to return, there are usually a number of signs. Common signs to watch for include:
- Moving
- Breathing
- Coughing
When ROSC occurs, the patient should have a palpable pulse and measurable blood pressure as well.
It is important to keep in mind that ROSC does not necessarily have to occur immediately during CPR. In some cases, it may even occur seconds or minutes after the cessation of CPR. This is called the Lazarus effect. Monitor patients closely for at least 10 minutes after ending CPR to watch for signs of ROSC.
What Increases the Chances of a Patient Experiencing ROSC?
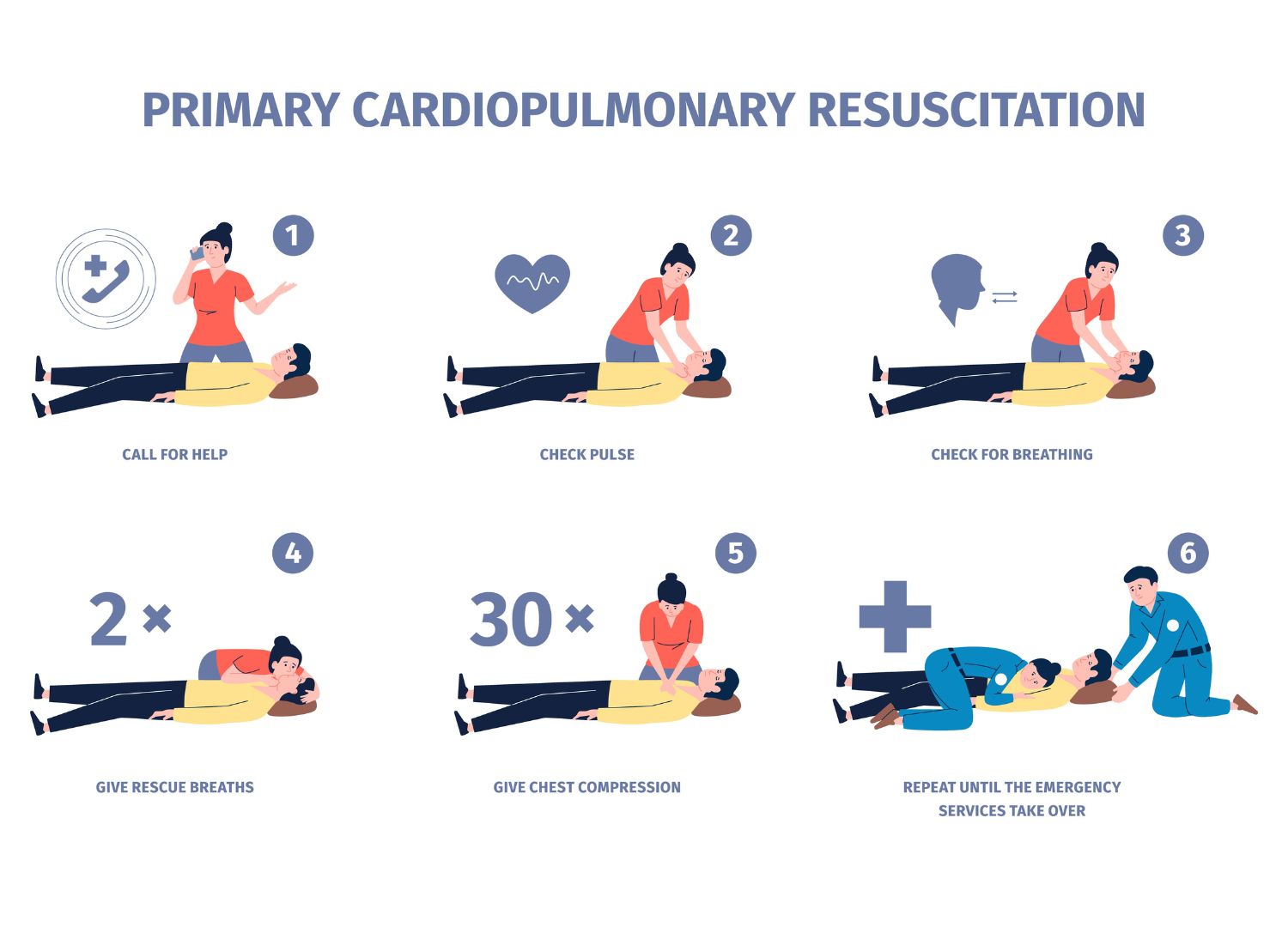
Patients are most likely to experience ROSC with cardiopulmonary resuscitation, defibrillation, or both, depending on the scenario. Achieving ROSC is a significant milestone for the patient, as the heart is beating on its own and is supporting the movement of oxygen around the body (to prevent further damage to the vital organs).
Factors that may affect the chances of patients experiencing ROSC include:
- How early cardiac arrest is recognized and how soon you initiate CPR. The sooner CPR begins, the better the chances are of maintaining the circulation necessary to oxygenate the organs.
- The overall quality of the CPR. The CPR given to the patient must be of the right quality to improve the chances of ROSC. Consistent chest compressions are a key component of successful CPR and should rarely, if ever, be interrupted throughout CPR. Defibrillation should be given to patients with ventricular fibrillation or arrest rhythms that require it. CPR and AED certification help ensure you have the tools you need to know what to do in this scenario.
- If you can provide the appropriate medications and life support while determining the underlying cause of the cardiac arrest. For example, the patient may require advanced cardiovascular life support (ACLS) including (but not limited to) epinephrine or airway management.
After treating a patient for cardiac arrest and ROSC occurs, post-resuscitation care is a key component of improving the chances of stabilizing the patient and their recovery. The exact care they need will depend on the length of the cardiac arrest and the reason for cardiac arrest.
How Soon Should ROSC Occur?
It’s important not to stop monitoring a patient even after you stop providing CPR or defibrillation efforts have failed. The reason for this is because of a condition called the Lazarus phenomenon.
The Lazarus phenomenon, better described as the “return to life from the afterlife,” was first described in 1982 by K. Linko. In 1993, it was given the name “the Lazarus phenomenon,” though you may know it best as auto resuscitation.
Auto resuscitation, spontaneous recovery after assumed death, has been reported many times in medical literature, and it is possible with patients who have delayed ROSC. The latest report of occurrences showed 76 cases of auto resuscitation across 27 countries through the end of 2022. So, while this is rare, it is not impossible.
What’s important to keep in mind about the Lazarus phenomenon is the conditions that may have led to auto resuscitation. In most cases, the patients didn’t have heart rhythms that were shockable. CPR was given, and in these cases, lasted from 6 to 90 minutes.
Cases of auto resuscitation have been reported 30 seconds post-CPR and up to as long as 180 minutes post-CPR. Most cases occur within a few minutes, so the official medical stance is to wait at least 10 minutes after the cessation of resuscitation procedures to confirm the patient’s death.
Does ROSC Predict a Positive Outcome for the Patient?
At the moment, ROSC is a positive sign, but it doesn’t mean the patient is out of harm’s way.
However, In ROSC medical literature, it’s shown that having ROSC itself doesn’t necessarily point to positive long-term outcomes. In reality, there are several factors that play a role in the likelihood of a positive outcome, including the duration of CPR. A Swedish cohort study from 2018 showed, for example, that out of 1,639 patients who experienced in-hospital cardiac arrest, 840 experienced ROSC and 471 survived for 30 days following it. Looking more closely, 768 of those patients had CPR. For those who needed only 3 to 5 minutes of CPR, the outcomes were better than for those who needed sustained CPR for anywhere from six to 60 minutes.
Taking Care of Patients Following ROSC
After successfully achieving ROSC, there are several steps you’ll want to take to encourage a better outcome for the patient.
Stabilizing the patient begins with ensuring their airways are open, oxygenation is occurring, and that they have adequate oxygen reaching the vital organs.
Some additional monitoring patients will need in the following hours and days post-cardiac arrest include:
- Glucose management: Glucose management is an important part of recovery after cardiac arrest, particularly in the case of working with someone with diabetes or other insulin-related illnesses. It’s appropriate to keep glucose controls between 81 and 180 mg/dL, depending on if the control has to be conventional or intensive.
- Temperature management: After cardiac arrest, it’s important to prevent fever if the patient is comatose. Preferably, the patient’s temperature will remain normal for at least 72 hours to reduce the risk of negative neurological outcomes.
- Electrocardiographic (ECG) monitoring: Electrocardiographic monitoring keeps a close watch on the heart’s rhythms and may help identify any arrhythmias or signs of other heart conditions that are leading to cardiac arrest or other heart problems.
- Blood pressure management: For patients who have gone into cardiac arrest, monitoring the mean arterial blood pressure is a necessity. Aim to keep it at 65 mmHg, not allowing the patient to be hyper or hypotensive.
- Airway management: Oxygenation is a vital part of protecting the patient’s organs. Adequate airway support may include mechanical support in some cases.
- Brain function monitoring: Particularly in the case of patients who have fallen unconscious or suffered a severe arrest, it’s necessary to keep a close eye on brain function. If they develop seizures, it could be a sign of anoxia and a lack of oxygen making it to the brain. In some cases, seizures are also a sign of a brain injury or brain death.
- Electrolyte monitoring: As a part of temperature management, and as a way of helping rebalance the cardiovascular system, it’s wise to provide patients with cold infusions of a balanced electrolyte or saline solution. Monitoring the patient’s bloodwork can also help identify when potassium, for example, is necessary to help during the patient’s recovery.
Will Patients With ROSC Develop Post-Cardiac Arrest Syndrome?
Post-cardiac arrest syndrome is a critical, complex condition that patients who have gone through cardiac arrest and been resuscitated develop. The severity of this condition can depend on several factors, but most patients will have some elements of it regardless of their age, the length of time the cardiac arrest lasted, and other elements.
Post-cardiac arrest syndrome includes ischemic-reperfusion injuries. These injuries occur across multiple organs as they begin to receive new blood flow, oxygen, and nutrients through spontaneous circulation. However, returning to normal function isn’t as simple as that, and these patients may need significant support to avoid going into shock and, in worst-case scenarios, passing away.
For example:
- Vasopressors may be needed to treat shock.
- Oxyhemoglobin saturation should be kept above 94%
- Strict temperature control, including therapeutic hypothermia in some cases, may be necessary to preserve the organs and brain function
Ischemia-reperfusion injuries are paradoxical, meaning they exacerbate the damage that has already been done despite the fact that the body is returning to its normal function. For that reason, patients have to be closely monitored following cardiac arrest, particularly if the arrest lasted for a significant amount of time. Reperfusion injuries can lead to irreversible tissue damage when muscle and tissue death have already begun. They can also lead to hypovolemic shock, acute renal failure, and lethal cardiac arrhythmias, which is why secondary cardiac arrest is possible even if a patient has successfully achieved ROSC.
Get CRP and AED Training To Improve the Odds of ROSC
ROSC is the goal of CPR, but to achieve it requires training in good technique and the appropriate use of CPR and AEDs. Get CPR and AED training through Save a Life by NHCPS.
Frequently Asked Questions
What Does ROSC Stand for?
ROSC is an abbreviation that stands for “Return of Spontaneous Circulation.” This represents the moment when cardiac function returns and respiration continues. ROSC indicates that the heart has started to beat again on its own and is effectively moving blood throughout the body. Oxygen, at this point, may also be moving around the body as long as the patient is also breathing on their own at that time.
ROSC is the goal of cardiopulmonary resuscitation (CPR) as well as advanced cardiovascular life support (ACLS). Take the free certification courses in CPR and ACLS through Save a Life by NHCPS to learn more about ROSC.
What Are Three Signs of ROSC?
There are many signs of ROSC, but the top three that you should be looking for when you’re working with a patient include physical signs such as coughing, moving, or breathing, measurable blood pressure, and a palpable pulse.
Do You Stop CPR If ROSC Occurs?
Once ROSC occurs, CPR can usually stop. However, you do need to monitor the patient carefully, as they may need additional medical support to continue to have good cardiac function on their own. For example, they may need epinephrine or other medications to handle the side effects of going into cardiac arrest, or they may need additional oxygen to support them on the way to the hospital.
If ROSC doesn’t occur or it occurs and then cardiac arrest happens again, remember that it’s appropriate to stop CPR only after 20 minutes if there is no establishment of the cardiac rhythm or sign of life.
What Is ROSC and Is It Associated With Positive Outcomes?
Unfortunately, while ROSC is a positive sign in the short term, it is not a predictor of the long-term outcome for patients. In some cases, patients do die after their circulation returns due to secondary cardiac arrest or other issues. A key to a successful outcome post-ROSC is continuing to provide support to stabilize the patient and then identifying the core cause for the cardiac arrest to begin with.
What Training Helps Improve the Chances of ROSC?
There are many kinds of training that can help improve the chances of patients achieving ROSC. Common strategies to implement include:
- The use of new technology. With technology such as advanced monitoring devices used during CPR, it’s easier to get real-time information about the patient. That includes minimal signs of life that may be missed with visual monitoring. Additionally, this technology can even give feedback on the quality of compressions.
- Quick access to AEDs. AEDs are found in many public spaces, making it simpler to use them when they’re needed. Additionally, the technology in these new devices can identify the appropriate time to shock the heart to (hopefully) get it back into rhythm. Having AEDs in workplaces, homes, and public places ensures they’re available when needed.
- Dispatcher-assisted CPR. When a family member or member of the public calls 911 for assistance, dispatcher-assisted CPR can help. Giving real-time instruction to the person performing CPR ensures they perform it as well as possible until a team of medical professionals can get to the scene.
- CPR and AED training for the public as well as medical professionals. You can get CPR and AED training through Save a Life by NHCPS.








Leave a Reply